Last Updated on August 28, 2025 by Doctors Supplement Store
GLP-1 Natural Alternatives: Supporting Metabolic Health Beyond Medications

GLP-1 Natural Alternatives: Supporting Metabolic Health Beyond Medications
GLP-1 Natural Alternatives: Supporting Metabolic Health Beyond Medications
GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) have transformed the landscape of type 2 diabetes and obesity care. Their effectiveness in promoting weight loss and glycemic control has garnered widespread attention—from celebrity headlines to clinical guidelines. But as more patients explore or discontinue these medications, functional and integrative medicine providers have a growing opportunity to offer complementary or alternative strategies that support similar metabolic pathways—often with fewer side effects.
What Are GLP-1 Agonists—and Why Are They So Popular?
GLP-1 (glucagon-like peptide-1) is an incretin hormone that stimulates insulin secretion, slows gastric emptying, and reduces appetite. Pharmacologic GLP-1 receptor agonists mimic this hormone, helping patients achieve significant weight loss and improved blood sugar regulation.
Recent trials have shown:
- Up to 20% body weight reduction with weekly GLP-1 agonists (Wilding et al., NEJM)
- Improvements in HbA1c, fasting glucose, and cardiovascular outcomes (Marso et al., NEJM)
This drug class is now widely used for:
- Obesity (with or without diabetes)
- Type 2 diabetes
- PCOS-related insulin resistance
- Metabolic syndrome
Common Side Effects and Patient Concerns
Despite their benefits, GLP-1 agonists are not without risks or drawbacks. Providers are increasingly seeing side effects such as:
- Nausea, vomiting, and delayed gastric emptying
- Fatigue and muscle loss during rapid weight loss
- Micronutrient depletion from reduced food intake
- Emotional dysregulation related to appetite and blood sugar swings
- Plateaus or weight regain after discontinuation
Some patients also feel disconnected from their hunger cues or experience anxiety about long-term dependency on injections.
Functional Medicine Opportunities: Beyond the Prescription
This is where functional medicine excels—by restoring foundational systems and helping the body regulate itself.
Providers can:
- Support nutrient repletion during caloric restriction
- Address muscle loss with mitochondrial and protein support
- Optimize insulin signaling with botanicals and minerals
- Improve gut function impacted by slowed motility
- Guide patients transitioning off medications with sustainable protocols
Natural Alternatives That Support GLP-1 Pathways
Several natural compounds can influence similar metabolic mechanisms as GLP-1 agonists, often with additional benefits:
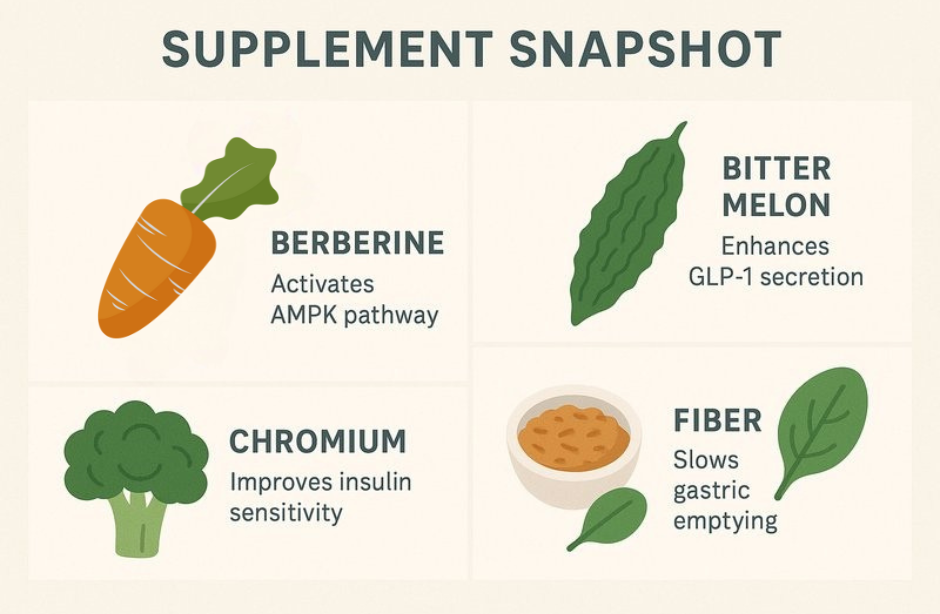
Supplement Snapshot
| Ingredient | Mechanism/Pathway | Key Benefit |
|---|---|---|
| Berberine | AMPK activation, gut GLP-1 signaling | Insulin sensitivity, weight support |
| Myo-Inositol | Insulin signaling | PCOS, glucose metabolism |
| Bitter Melon | Insulin mimetic | Lowers fasting glucose, HbA1c |
| Chromium | Enhances insulin receptor activity | Blood sugar balance, cravings |
| Fiber Blends | Slows gastric emptying | Appetite, glycemic control |
| Adaptogens | Cortisol regulation | Energy, stress resilience |
Providers can also highlight lifestyle “biohacks” known to boost natural GLP-1, such as exercise, circadian alignment, and prebiotic-rich foods.
Clinical Pearls: Supporting Patients On or Coming Off GLP-1 Drugs
Functional providers are uniquely positioned to support patients tapering off GLP-1s or managing post-medication metabolism.
Tapering Considerations:
- Gradually reduce GLP-1 dosing while increasing fiber and protein intake
- Begin nutraceutical support (e.g., berberine, chromium) 2–4 weeks prior to taper
- Monitor lean mass and glycemic variability
- Support appetite signaling with mindful eating and circadian regulation
- Address gut motility and emotional eating patterns with botanical support
Clinical Example: A Case in Practice
A 52-year-old female on semaglutide for 6 months presented with nausea, fatigue, and concern about lean mass loss. Her provider implemented a mitochondrial support protocol (CoQ10 + carnitine + magnesium), increased protein intake, and layered in berberine. Within 8 weeks, energy improved, nausea resolved, and DEXA confirmed preservation of lean mass.
Personalizing the Approach: Protocols That Work
Functional providers can create tailored plans using:
- Supplement protocols to support appetite, energy, and blood sugar
- High-protein, nutrient-dense meals to prevent lean mass loss
- Time-restricted eating for glycemic control and satiety
- Movement prescriptions for muscle preservation and mitochondrial health
- Gut support for motility and microbiome balance
These strategies help patients experience sustainable results—whether they’re on GLP-1 meds, tapering off, or looking for a more natural path from the start.
🔍 Looking for GLP-1 Support Supplements?
Browse berberine, mitochondrial blends, and professional-grade fiber formulas in your DSS dispensary—or contact us to build a personalized protocol for your patients.
Practical Takeaway
Patients are looking for options. When providers combine science-backed natural interventions with personalized care, they become trusted guides through a complex metabolic journey.
Recent Articles
Creatine and Cognition: Is There Benefit for Alzheimer’s Disease?
Source: Today’s PractitionerThe Creatine to Augment Bioenergetics in Alzheimer’s (CABA) trial is a single-arm pilot trial published in Alzheimer’s & Dementia Translational Research & Clinical Interventions. Twenty patients meeting the McKhann criteria for...


