Factoring in Exposure to Mold and Mycotoxins
Factoring in Exposure to Mold and Mycotoxins
Author: Dr. Matt Hyatt-Pratt, PhD
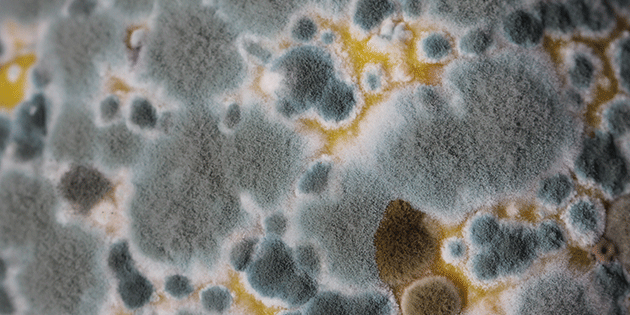
Due to genetic and environmental variation, symptoms and damage from exposure to mold and mycotoxins can be quite different from person to person. And because of the variability of symptoms (even within the same family) mold and mycotoxin exposure can often go undiagnosed. Common bodily damage is associated with mold and mycotoxin exposure. These microbes can have an intense effect on human immunity when exposed. Learn how to spot symptoms and know when to use testing.
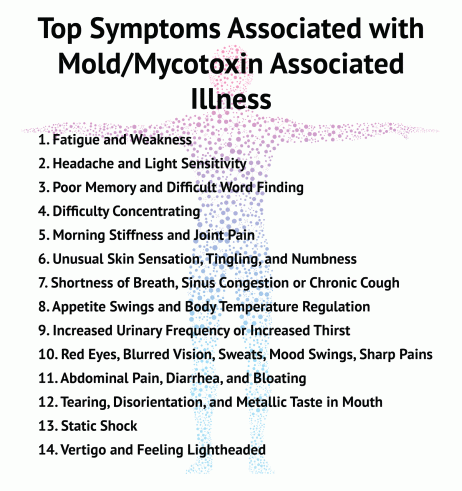
Common symptoms that may arise are fatigue, headaches, poor memory, abdominal pain, vertigo, etc (Figure 1)
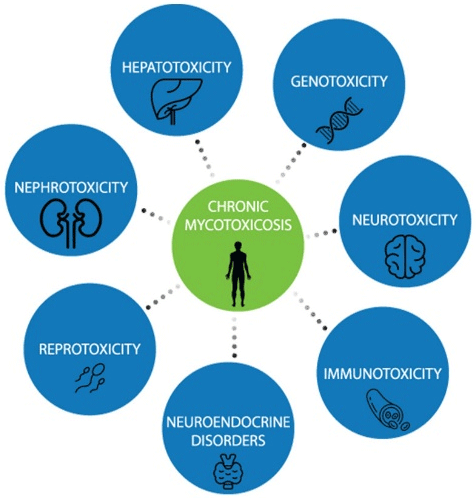
It’s problematic that many practitioners are not aware mycotoxins can cause many different types of ailments and can contribute to many different chronic illnesses. The bodily systems that are most commonly affected are: immune system, nervous system/brain, and gut (figure 2).
Through my studies and experience I have learned that most of the toxic mycotoxins effect the immune system in some way. Mycotoxins have even been commercialized by the pharmaceutical industry as a immunosuppressant medication (CellCept and Myfortic), which can be used to prevent organ donation rejection, and treat lupus, rheumatoid arthritis, and other autoimmune disease (1). Many other mycotoxins can cause immune suppression such as gliotoxin, aflatoxin, and trichothecenes (2-4). This suppression of the immune system can lead to other infections including bacterial, viral, and fungal. These infections can occur throughout the body but are especially localize in the gut and respiratory tract (common spots of mold colonization) (5). These infections can make the diagnosis of mold and mycotoxins even harder to pin down, because practitioners are distracted by these infections and don’t know to dig deeper for underlying causes. I frequently consult with practitioners whose patients have had multiple cases of bacterial or fungal overgrowth before finding out the underlying problem of mycotoxins. I suspect, however with no data to substantiate, that a significant amount of Lyme patients have significant mycotoxins. It is my hypothesis that if we measured mycotoxins in a large population of Lyme patients, they would have higher amounts than the general public. It is these higher amounts of mycotoxins that allow for the overgrowth of the pathogenic bacteria.
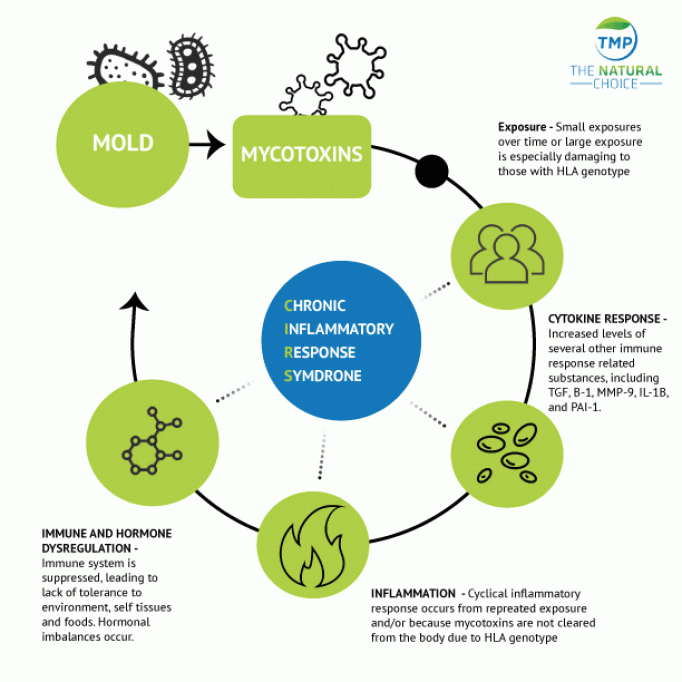
Unfortunately, immune suppression is not the only immune response caused by mold and mycotoxins. The immune system can be fall into an out-of-control cascade when mold and mycotoxins exposure increases circulating plasma chemokine and cytokine levels (6). These reactions can be triggered by both allergen dependent and independent mechanisms (7). Inflammation can lead to many of the symptoms associated with mold and mycotoxin exposure. Some of the most important symptoms are associated with the respiratory tract. Mold exposure has been linked to a nine-fold increase in emergency room visits among asthmatics (8). These phenomena are tied to alterations in inflammatory system pathways. Data indicate that several cytokines are elevated when patients are exposed to mold and mycotoxins. These include IL-17, IL-10, TGF-α, and MIP-1β (6). This inflammation has been referred to as CIRS (Chronic Inflammatory Response Syndrome) (Figure 3).
“the take home message is that gut issues are a common hallmark of mold and mycotoxin exposure”
When mold exposure is involved, likely the most common symptoms driving patients to seek medical help pertain to neurological symptoms. Recent studies have tied exposure to mold and mycotoxins to many different types of neurological problems. Some of the more common issues are headaches, migraines, Parkinson’s, multiple sclerosis, and Alzheimer’s(9-12). However, this is nowhere near a complete list. Many of these diseases have been tied to inflammation. Mycotoxins trigger multiple different pathways which can lead to induced apoptosis. T-2 and trichothecenes enter cells and trigger expression of MEKK1 and c-jun and the downregulation of Nrf2(13, 14). These changes will lead to increased oxidative stress and decreased detoxification. Ochratoxin (OTA) has a much more complex method for damaging neuronal cells. Multiple papers indicate a mixture of oxidative stress, inhibition of protein synthesis, and OTA induced DNA breaks can lead to damage to the neuronal system (15, 16). As disconcerting as these results are, there is a lot of hope in the newest research. There are newer studies showing neurological decline can be reversed if the toxin source can be located and treatment is performed (17).
Though I spend more time on gut issues in another blog post, the take home message is that gut issues are a common hallmark of mold and mycotoxin exposure. I frequently consult with practitioners and their patients that suffer from leaky gut and increased food sensitivities. If your patient is having frequent gut pain and not responding to current treatment, it might be time to consider the potential of exposure to mold and mycotoxins.
Shared with permission from Dr. Matt Pratt-Hyatt. For additional information on this subject related to proper environmental testing as well as the primary types of clinical tests available check out Dr. Matt Pratt-Hyatt’s blog at themoldpros.com.
Dr. Matt Pratt-Hyatt, PhD is the Director of Research and Business Development at The Mold Pros.
He has been in the toxin field for 12 over years and has been in functional/integrative/alternative medicine for over eight years. He received his PhD in 2008 from the University of Michigan and received additional training in the labs of Paul Hollenberg and Curtis Klaassen, where he learned about toxins and how the body eliminates them.


